Introduction: Immune-mediated inflammatory diseases (IMIDs) constitute a clinically heterogeneous group with a disruption of the immune system that provokes inflammation of any organ system on a chronic basis. Previous observational investigations have demonstrated an association between a person's or their family's medical background of IMIDs and a higher likelihood of developing Hodgkin's lymphoma (HL). Nevertheless, the exact causal connection between specific IMIDs and HL remains ambiguous. Therefore, the investigation aims to explore the causal effects between IMIDs and HL.
Methods: A two-sample Mendelian randomization (TSMR) approach was employed in this study, using publicly available genome-wide association study summary statistics. The inverse variance weighted (IVW) method was the primary approach used for the Mendelian randomization (MR) analysis. Furthermore, supplementary statistical approaches such as MR-Egger, simple mode, weighted median, and MR-PRESSO were employed. In order to identify potential heterogeneity and pleiotropy, several tests were conducted, including Cochran's Q test, the MR-Egger regression test, and the MR-PRESSO test. Moreover, the leave-one-out method was implemented to examine the reliability of the MR results.
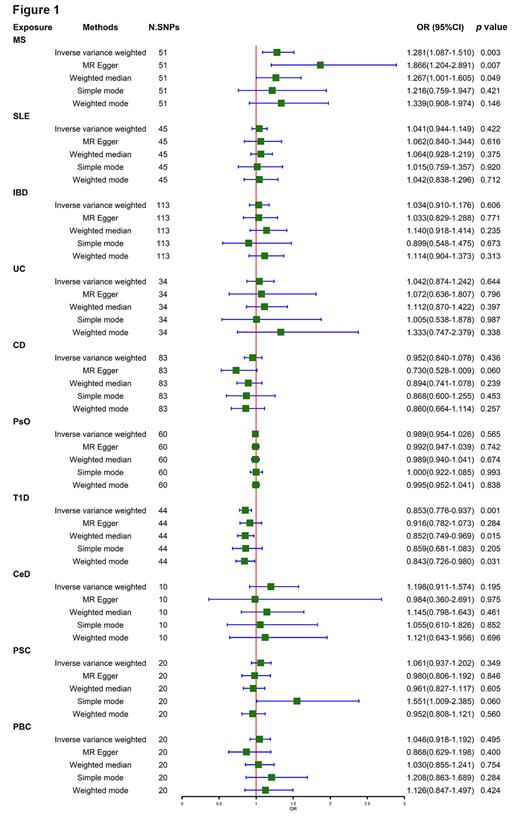
Results: Based on the IVW analysis the findings revealed a positive causal link at risk for multiple sclerosis (MS) and HL [odds ratio (OR) = 1.281; 95% CI = 1.087-1.510, p = 0. 003] and a negative causal link at risk for type 1 diabetes (T1D) and HL (OR = 0.853; 95% CI = 0.776-0.937, p = 0.001). However, no significant causal relationship was found between the risk of HL and the other eight IMIDs, including inflammatory bowel diseases (OR = 1.034; 95%CI = 0.910-1.176, p = 0.606), systemic lupus erythematosus (OR = 1.041; 95%CI = 0.944-1.149, p = 0.422), Crohn's disease (OR = 0.952; 95%CI = 1.840-1.078, p = 0.436), ulcerative colitis (OR = 1.042; 95%CI = 0.874-1.242, p = 0.644), primary sclerosing cholangitis (OR = 1.061; 95%CI = 0.937-1.202, p = 0.349), primary biliary cirrhosis (OR = 1.046; 95%CI = 0.918-1.192, p = 0.495), psoriasis (OR = 0.989; 95%CI = 0.954-1.026, p = 0.565), celiac disease (OR = 1.198; 95%CI = 0.911-1.574, p = 0.195). Figure 1 displayed a detailed visual representation of the findings obtained in the study. No indication was made of any potential heterogeneity or horizontal pleiotropy. Besides, no outliers were discovered in the MR using MR-PRESSO. In addition, the leave-one-out analysis indicates that the MR estimates are not driven by any single SNP, suggesting that the observed associations are robust and reliable.
Conclusions: The present investigation emphasizes an increased susceptibility of MS to the risk of HL and a potential protective effect of T1D against the risk of HL. In light of these findings, patients with MS receiving immunosuppressive therapy are highly suggested to undergo periodic physical evaluations and lymphoma surveillance. Further investigations are warranted to explore the potential mechanisms of MS and T1D on the development of HL.
Disclosures
No relevant conflicts of interest to declare.